Myasthenia Gravis
What Is Myasthenia Gravis?
Myasthenia gravis is a rare, chronic autoimmune neuromuscular disease characterized by muscle weakness and muscle fatigue in the body’s voluntary muscles. Autoimmune diseases cause the body’s immune system to attack its own tissues. Myasthenia gravis may affect one muscle group, such as the eyes, or multiple muscle groups all over the body.
Thoracic surgeons often encounter and treat myasthenia gravis because the thymus gland, which produces some of the immune chemicals that cause the condition, is located in the chest, below the throat. Removing the thymus gland—a procedure known as thymectomy—is a mainstay in the surgical treatment of myasthenia gravis.
Myasthenia Gravis and the Thymus Gland
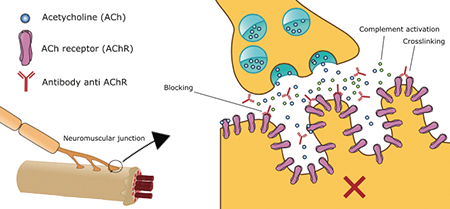
In myasthenia gravis, communication between the nerve and muscle is interrupted and the muscle is prevented from contracting. Specifically, the antibodies destroy acetylcholine—a neurotransmitter that tells muscles to contract—receptor sites faster than the body can create new ones. As receptor sites become depleted, the muscles cannot be activated and function as they should.
There are some individuals that product antibodies to various other proteins instead of acetylcholine, which can also interrupt transmission of the nerve signal.
Role of the thymus gland
The thymus gland secretes many hormones and is associated more with the immune system than the endocrine system. One of the hormones the thymus produces is necessary for the production of T-cells, an important type of white blood cell that protect the body against both infectious disease and foreign invaders.
Researchers believe the thymus gland triggers or possibly maintains the production of the antibodies that block the neurotransmitter acetylcholine. In many people with myasthenia gravis, the thymus gland is abnormally large.
Types of Myasthenia Gravis
Myasthenia gravis is categorized into subdivisions, including the following, though there are more specific forms:
- Ocular myasthenia gravis – affects the muscles of the eyes
- Generalized myasthenia gravis – involves multiple muscle groups
- Congenital myasthenia gravis – caused by defective genes (not autoimmune, as in other forms); usually has onset at or near birth, but it can appear later in childhood or adulthood
- Transient neonatal myasthenia gravis – rare, temporary form affecting infants born to mothers with myasthenia gravis, usually lasting a couple months
- Juvenile myasthenia gravis – rare childhood form; onset before age 19 with distinct symptoms differing from adult myasthenia gravis
Symptoms
Symptoms of myasthenia gravis vary depending on the type of disease and the individual patient. Symptoms may include:
- Ptosis – weakness and drooping of the eyelids, which is the most common symptom and present in most forms, making it a distinguishing factor of the disease
- Diplopia – double vision caused by weakness of eye muscles
- Dysarthria – impaired speech
- Dysphagia – difficulty chewing and swallowing
- Excessive muscle fatigue following activity
- Proximal limb weakness – weakness of the upper arms and legs
In about 10 percent of patients, affected individuals may develop myasthenic crisis, which is a potentially life-threatening situation. In myasthenic crisis, complications due to severe involvement of muscles of the respiratory system used during breathing occur. This is an emergency situation.
Myasthenia gravis symptoms can worsen with stress, illness, physical fatigue and certain medications. Symptoms can be remitting, meaning they come and go, and the duration of remission is variable. In some cases, patients may go into remission permanently. Though they still have the disease, they become asymptomatic.
Causes and risk factors
There are no known risk factors for myasthenia gravis. The disease affects men, women, children, all races and ethnic groups. There is a high incidence of disease in women between the ages of 20 and 40 and men over the age of 60, however the disease can present at any age. Myasthenia gravis is not contagious, nor is it hereditary, though it may occur in more than one member of the same family.
Diagnosis
The diagnosis of MG can be difficult, as the initial symptoms can be subtle and similar to other autoimmune and neurological disorders. The characteristic symptoms include fatigability and muscle weakness, which improves with rest but worsens again quickly with repeat exertion. The affected muscles can include the eyes, limbs, axial (or trunk) or in some cases respiratory muscles. Other symptoms that can indicate MG are difficulty swallowing, slurred speech, unstable gait and a droopy eye.
Often diagnosis is confirmed with a patient’s response to medications that act to reduce the blocking action of the autoantibody. In many cases of myasthenia gravis, radiologic evaluation (i.e. CT scan) can reveal an abnormality of the thymus gland.
Treatment
Although there is no known cure for myasthenia gravis, there are many treatments that control symptoms and allow for a high quality of life. Most patients with this disease have a normal life expectancy.
Standard treatment for myasthenia gravis usually begins with medication, typically an acetylcholinesterase inhibitor. This type of medication acts to prolong the life of acetylcholine and provide temporary symptomatic relief of muscle weakness. It is often coupled with immunosuppressive drugs to reduce the autoimmune response. Unfortunately, over time, many drug regimens for myasthenia gravis lose their effectiveness and may cause severe side effects.
Thymectomy
The surgical treatment for MG involves the removal of the thymus gland (thymectomy). The thymus gland plays a major role in developing the immune system during infancy and childhood. As an adult, there is very little thymic function; the gland actually reduces in size and becomes replaced by fatty tissue. Successful removal of the entire gland has shown to be more than 95 percent effective in improvement of the disease. Studies suggest that approximately 80 percent of patients experience complete resolution of symptoms after surgery with more than half able to come off all medications.
The surgical management of myasthenia gravis has a long track record of success, dating back to 1941 at Johns Hopkins and first performed by Dr. Alfred Blalock. The surgical treatment for myasthenia gravis involves the removal of the thymus gland.
Thoracic Group Approach to Surgical Treatment of MG
Thoracic Group approaches the surgical treatment of MG with a team effort, from the pre-operative evaluation to the operating room and recovery, to optimize outcomes and our patient’s experience. The optimal surgical approach to the removal of the thymus gland is a VATS thymectomy.
Thoracic Group surgeons are world renowned chest surgeons with superior experience in the specialty of video-assisted thoracic surgery (VATS), a minimally invasive approach to surgery in the chest.
The team approach to surgical treatment of MG starts with the coordination of the multidisciplinary team of physicians that care for patients with this disorder. Thoracic Group surgeons confer with neurologists, pulmonary specialists, and anesthesiologists throughout the peri-operative course in regard to indication for surgery, risk assessment and management.
The team approach extends to the operating room, where Dr. Bocage and his team perform all surgical procedures together. Specialized anesthesiologists, highly skilled OR nurses and knowledgeable patient navigators round out the team during the course of pre-operative preparation, the operation itself and recovery.
Patients undergoing a VATS thymectomy report to the hospital on the morning of surgery and typically go home the following day. Full recovery at home is usually achieved within two weeks of the procedure.
Why is VATS Thymectomy the Preferred Approach?
There are many advantages of VATS thymectomy over a traditional open approach (i.e. sternotomy):
- Less pain
- Lower complication rate
- Lower risk of infection
- Shorter operative time thus less anesthesia
- Shorter hospital stay and decreased recovery time
The benefits of a minimally invasive approach over traditional surgery are even more important in MG patients because of the already compromised immune state. Postoperative complications and infection are drastically reduced with VATS. Additionally, the VATS approach creates markedly reduced trauma to respiratory muscles and structures (chest wall) when compared with traditional open surgery.
If you have myasthenia gravis and believe a thymectomy could help, request an appointment at Thoracic Group. We will provide all the information you need to make an informed decision, and we will schedule your surgery if you are a good candidate.
Treatment for Myasthenia Gravis
Standard treatment for MG usually begins with medication, typically an acetylcholinesterase inhibitor. It acts to prolong the life of the neurotransmitter (acetylcholine) and provide temporary symptomatic relief of muscle weakness. Immunosuppressive drugs are often added to the regimen to reduce the autoimmune response. Unfortunately, over time, most drug regimens lose their effectiveness and may cause severe side effects.
The surgical management of MG has a long track record of success, dating back to 1941 at Johns Hopkins and first performed by Dr. Alfred Blalock. The surgical treatment for MG involves the removal of the thymus gland (thymectomy). The thymus gland plays a major role in developing the immune system during infancy and childhood. As an adult, however, there is very little thymic function; the gland actually reduces in size and becomes replaced by fatty tissue. A portion of patients with MG has a tumor on the thymus gland. This tumor is known as a thymoma, and can either be benign or malignant.
The thymus gland in an adult can be removed with no ill effects. Successful removal of the entire gland has shown to be more than 95% effective in improvement of the disease. Studies show that approximately 80% of patients experience complete resolution of symptoms after surgery with more than half able to come off all medications.
Patients undergoing a VATS (video assisted thoracic surgery) thymectomy report to the hospital on the morning of surgery and typically go home the following day. Full recovery is usually achieved within two weeks of the procedure.
[contact-form-7 id=”2995″ title=”Subpage contact form”]
